Factors for a lower segment cesarean section (LSCS) include maternal conditions like obesity, hypertension, and diabetes, as well as fetal issues such as distress, malpresentation (breech or transverse lie), or multiple pregnancies. Other factors include previous LSCS, a prolonged or stalled labor, failed induction, or placental problems like placenta previa.
Maternal factors
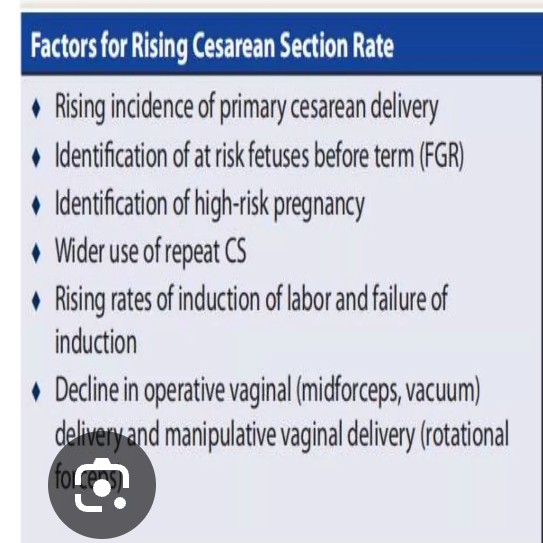
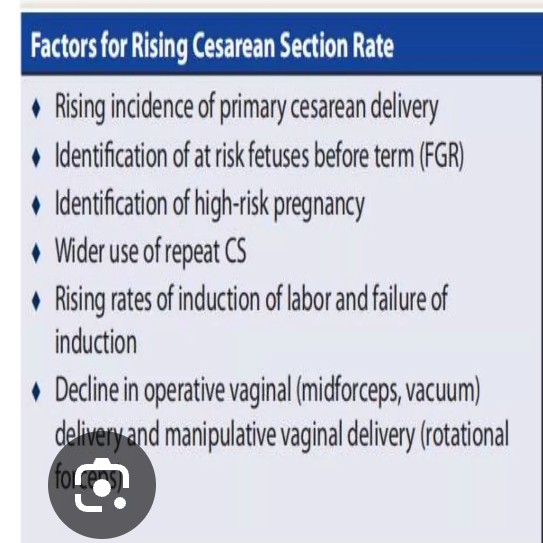
Previous LSCS: A prior cesarean is a leading reason for a repeat LSCS.
Maternal health conditions: Pregnancy-induced hypertension, gestational diabetes, and obesity are significant risk factors.
Placental problems: Conditions where the placenta blocks the cervix, such as placenta previa, necessitate a cesarean.
Failed induction: An induction of labor that does not progress can lead to an LSCS.
Multiple pregnancies: Having twins, triplets, or more babies, especially if the first twin is not head-down, is a risk factor.
Prolonged or stalled labor: A labor that is slow to progress or stops can be an indication for LSCS.
Fetal factors
Fetal distress: A sign that the baby is not tolerating labor can prompt an LSCS.
Malpresentation: The baby is not in a head-down position, such as being breech (feet or buttocks first) or in a transverse (sideways) lie.
Cord prolapse: The umbilical cord comes out of the uterus before the baby, which is an emergency and requires an immediate cesarean.
Other factors
Urgency: Some indications, like fetal distress or cord prolapse, lead to an emergency LSCS.
Elective timing: Other factors, such as a planned LSCS for a non-emergency reason like a previous LSCS or a persistent breech presentation, are sometimes scheduled in advance.